Abstract
Background: Methotrexate (MTX) is a critical component of combination chemotherapy treatment for pediatric patients with acute lymphoblastic leukemia (ALL). MTX is an antimetabolite often administered intravenously in high doses (HD) requiring hospital admission alongside intravenous fluids and concurrent treatment with a MTX antidote until HDMTX excretion reaches a safe level. Delayed clearance and prolonged exposure to HDMTX can increase the likelihood of life-threatening adverse events (AEs) including mucositis, kidney injury, pleural effusion, neurotoxicity, kidney injury, neutropenia, and thrombocytopenia. Further research is needed to evaluate the relationship between delayed HDMTX clearance and AEs and to explore the association between demographic factors and delayed HDMTX clearance.
Objective: The main objective of this study was to model concentrations of HDMTX over time and analyze differences in severe AEs associated with increased HDMTX concentration.
Methods: This is a multi-center retrospective cohort study conducted at Children's Healthcare of Atlanta, Cincinnati Children's Hospital Medical Center, and Texas Children's Hospital. Local institutional review board approval was obtained by each center. Eligibility included children with ALL aged 0-21 years at diagnosis who received at least one dose of HDMTX (defined as ≥ 500 mg/m2) at a participating institution from January 2010 through December 2020. Demographics (age at diagnosis, sex, race, ethnicity) and clinical factors (vital status, HDMTX concentration relative to timing of infusion, and AEs) were abstracted or extracted from the electronic health record. The following AEs were identified from each HDMTX administration to subsequent chemotherapy: mucositis, elevated creatinine, pleural effusion, neurotoxicity, neutropenia, and thrombocytopenia. AEs were graded using Common Terminology Criteria for Adverse Events v5 definitions. Only grade 4 neutropenia and grades 3-4 thrombocytopenia were collected. Methotrexate concentrations at exactly 24, 36, 42, 48, 60, and 72 hours were estimated after fitting data to a three compartment pharmacokinetic model using NONMEM. Area under the curve (AUC) was estimated with Edsim++. Descriptive and inferential statistics were calculated including generalized estimating equations (GEE) to assess the association between HDMTX concentrations and exposure (AUC) and each toxicity and to analyze risk factors including age, sex, race, and ethnicity for HDMTX concentrations in univariate analyses. All analyses were completed using SAS 9.4.
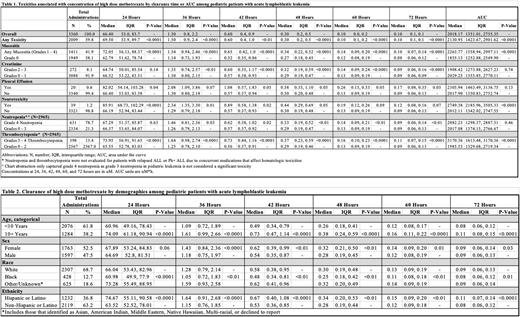
Results: There were 3,360 HDMTX administrations from 926 patients in the analysis. Median age was 7.8 years, and more patients were female (57.8%). The cohort was diverse (white: 67.7%, black: 12.7%; Hispanic/Latino: 38.0%, Non-Hispanic/Latino: 62.0%). Table 1 describes associations between elevated MTX concentrations at different time points and AEs. Neutropenia (78.7%) and any grade mucositis (41.9%) were the most common AEs. Development of mucositis or thrombocytopenia was associated with elevated MTX concentrations at all time points and AUC, while any grade neurotoxicity was more closely associated with early concentrations. Neutropenia and creatinine increase were not associated with elevated early concentrations or AUC, but development of these AEs was associated with elevated concentrations on or after 42 hours. Pleural effusions were rare and marginally associated with higher concentrations. Patients aged 10+ years had higher concentrations at all timepoints and female patients had slightly higher concentrations at most time points. Black patients had lower concentrations and Hispanic patients had higher concentrations at all timepoints (Table 2).
Conclusion: Elevated concentrations of MTX may be associated with development of AEs, but the relationships vary by AE. Elevated MTX concentrations at any time point are associated with development of mucositis and thrombocytopenia, but the association with other AEs changes depending on timing of MTX concentration elevation. There are clear differences in MTX concentrations by demographics. These results highlight who may be at risk for toxicities and require additional supportive care. Work is ongoing to incorporate clinical characteristics and concentration at each time point into joint models to evaluate risk of methotrexate-induced AEs.
Disclosures
Miller:BTG Specialty Pharmaceuticals: Research Funding. Bernhardt:BTG Specialty Pharmaceuticals: Research Funding. Ramsey:BTG Specialty Pharmaceuticals: Honoraria, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal